One of the most vital aspects of managing diabetes is regular blood sugar monitoring. This simple yet effective practice is crucial for keeping diabetes under control, preventing complications, and ensuring overall health. Whether newly diagnosed or managing diabetes for years, understanding the importance of consistent monitoring is key to a successful management plan.
1. Helps Prevent Dangerous Blood Sugar Fluctuations
Regular blood sugar monitoring helps prevent sudden fluctuations in blood sugar levels. Diabetes often involves the body’s inability to properly regulate glucose, and without consistent monitoring, it can be difficult to recognize when blood sugar becomes dangerously high (hyperglycemia) or low (hypoglycemia), both of which can lead to serious health issues.
- Tip: By regularly checking your blood sugar, you can detect trends and patterns, allowing for timely adjustments to your treatment plan.
2. Allows for Better Decision Making
Managing diabetes isn’t just about taking medication or insulin; it’s also about making informed decisions regarding diet, exercise, and lifestyle. Monitoring blood sugar provides insight into how foods, activities, and medications impact glucose levels, helping make personalized choices for better control.
- Tip: Keep a record of your readings and discuss them with a healthcare provider to tailor a care plan and make necessary adjustments.
3. Prevents Long-Term Complications
Consistent monitoring is important for preventing long-term complications, such as nerve damage, kidney disease, heart disease, and vision problems. Keeping blood sugar levels within a target range minimizes the risk of these issues and helps ensure healthy organ function.
- Tip: Tight control of blood sugar, achieved through regular monitoring, is shown to reduce the risk of long-term diabetes-related complications.
4. Empowers You to Take Control of Your Health
Regular blood sugar monitoring empowers individuals to take control of their health. By understanding how the body responds to various factors, it becomes easier to actively participate in care, making better choices for long-term health.
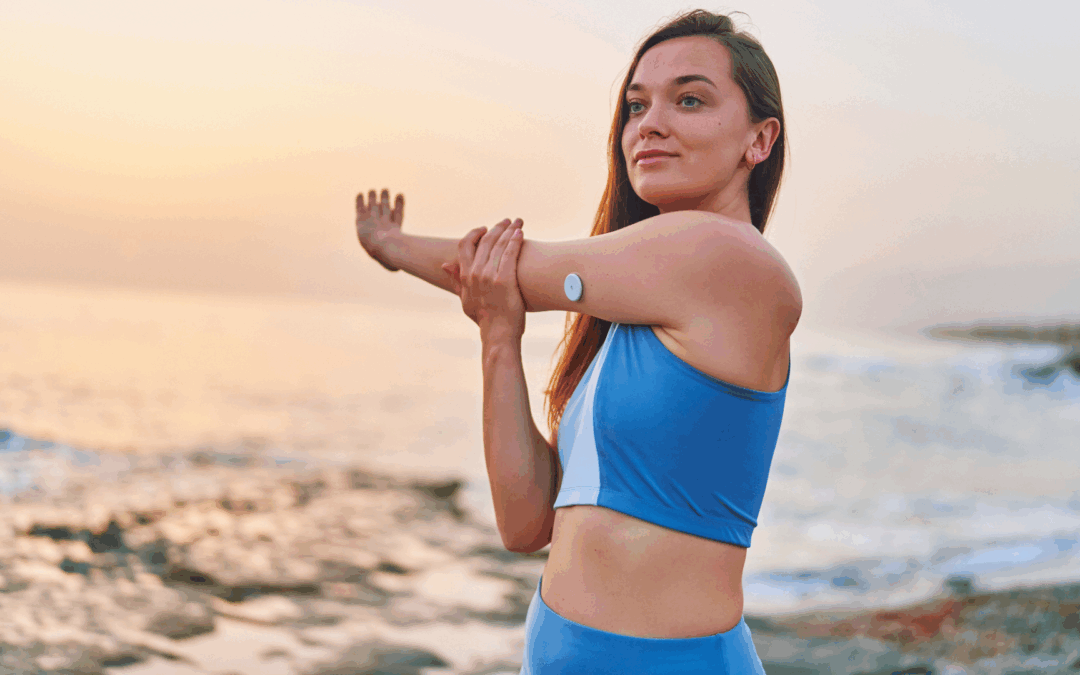
- Tip: Use continuous glucose monitors (CGMs) or home glucometers to track glucose in real-time. This helps make proactive adjustments to your lifestyle.
5. Improves Communication with Your Healthcare Team
Regular monitoring provides healthcare providers with accurate, up-to-date information to understand how well a diabetes management plan is working and make informed adjustments to treatment.
- Tip: Share blood sugar readings during appointments and note any changes in routine or symptoms to help fine-tune diabetes management.
6. Helps Prevent Hypoglycemia
Low blood sugar (hypoglycemia) is a common concern for many individuals with diabetes, especially those on insulin or certain oral medications. Regular monitoring helps detect early signs of hypoglycemia before it becomes dangerous, allowing immediate action such as consuming glucose or adjusting medication.
- Tip: If you experience symptoms like dizziness, shakiness, or sweating, check your blood sugar right away. If it’s low, treat it immediately with a fast-acting carbohydrate.
7. Provides Insight into Meal Timing and Composition
For people with diabetes, food plays a major role in blood sugar control. Tracking blood sugar before and after meals helps identify how certain foods or meal patterns affect glucose levels, providing valuable information for better control.
- Tip: Aim to monitor blood sugar before meals, 2 hours after eating, and at bedtime to understand the impact of meals on blood sugar levels.
8. Encourages Consistency and Discipline
Diabetes requires consistency and discipline. Regular blood sugar monitoring helps maintain this discipline by providing real-time feedback. Knowing that blood sugar levels will be checked can motivate individuals to stay consistent with medication, exercise, and dietary choices.
- Tip: Set reminders on your phone or calendar to check blood sugar at the same times each day for consistency.
If you’re unsure about how to begin monitoring blood sugar, talk to a healthcare provider for guidance on using a glucometer, when to test, and how often. Remember, the more informed you are, the better your chances of successfully managing your diabetes.
Important Note:
This content is for informational and educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider with any questions regarding a medical condition or treatment plan. No doctor-patient relationship is established by reading or interacting with this content.
You Might Also Like

How to Live Well with Type 2 Diabetes
When Lisa was diagnosed with type 2 diabetes, she felt like her life was being put on hold. She had always been active—she loved hiking, biking, and trying new recipes—but the diagnosis made...

10 Easy and Delicious Diabetic-Friendly Recipes to Try
When Mark was diagnosed with type 2 diabetes, he knew he had to make some serious changes to his lifestyle. But one of the hardest things to accept was the idea of giving up his favorite foods. He...
From Struggle to Strength: Sarah’s Journey to Managing Her Diabetes
Sarah was just 30 when her world turned upside down. She had always been the picture of health—she ran 5Ks, cooked fresh meals, and enjoyed a lifestyle that felt unstoppable. So, when her doctor...



